Genital Warts: Causes, Symptoms, and the Most Effective Treatments
What Are Genital Warts?
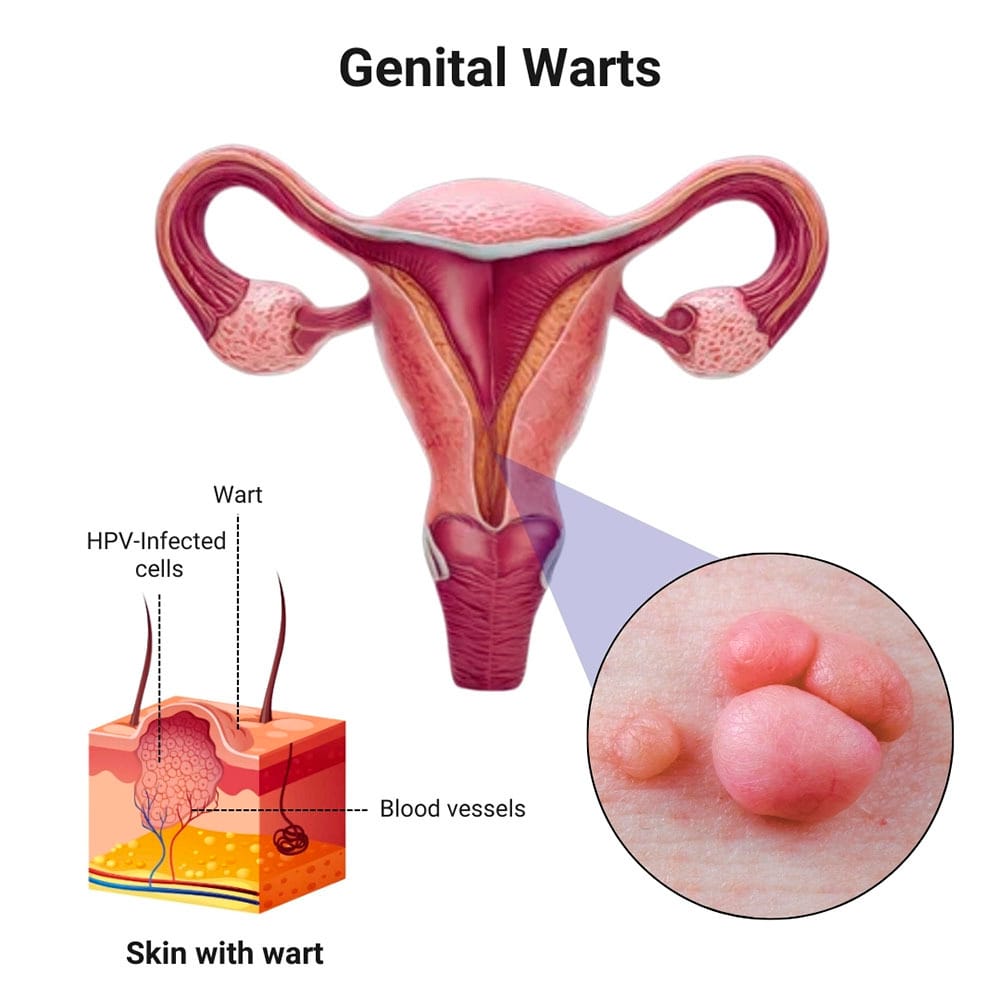
Genital warts are one of the most common types of sexually transmitted infections (STIs), caused by the human papillomavirus (HPV) — particularly HPV types 6 and 11. These warts appear as small, skin-coloured or grey growths in the genital and anal areas.
Though they are typically non-cancerous, genital warts can cause discomfort, itching, emotional stress, and recurrence. Early diagnosis and proper treatment are essential to control the spread and prevent complications.
What Causes Genital Warts?
Genital warts are spread through direct skin to skin contact during vaginal, anal, or oral sex with an infected person. Even without visible warts, an infected person can still transmit the virus.
Risk factors include:
- Multiple sexual partners
- Early initiation of sexual activity
- Weakened immune system
- Lack of condom use
- Previous history of STIs
Symptoms of Genital Warts
Genital warts can appear weeks or months after HPV exposure. Common signs and symptoms include:
- Small, soft, flesh-colored bumps
- Clusters that resemble a cauliflower
- Itching, discomfort, or slight bleeding
- Flat lesions in moist areas
- Warts on the vulva, vagina, cervix, penis, scrotum, anus, or thighs
Some individuals may have no visible signs but still carry and transmit the virus.
How Are Genital Warts Diagnosed?
Genital warts are usually diagnosed during a clinical examination by a dermatologist, gynecologist, or urologist. Additional diagnostic tools may include:
- Colposcopy to identify internal warts, especially in women
- HPV DNA testing in cases of abnormal Pap smears or suspected high-risk HPV types
Are Genital Warts Dangerous?
Warts caused by HPV types 6 and 11 are considered low-risk and are not associated with cancer. However, other high-risk HPV types (like 16 and 18) can cause cervical, anal, penile, or throat cancers. This makes HPV vaccination and routine screening important, especially for women.
Best Treatment Options for Genital Warts
While there is no cure for HPV, several treatment options are available to remove visible warts, relieve symptoms, and reduce recurrence.
- Topical Treatments
- Imiquimod (Aldara): Stimulates the immune system to fight the virus.
- Podophyllotoxin (Condyline): Destroys wart tissue; not suitable for pregnant women.
- Sinecatechins (Veregen): A botanical ointment derived from green tea extract.
Suitable for: Small, external genital warts
Treatment duration: 4 to 8 weeks, depending on the medication
- Cryotherapy (Freezing)
- Uses liquid nitrogen to freeze and destroy wart tissue.
- Causes the wart to blister and fall off over several days.
Advantages: Safe, quick, suitable for external warts
Limitations: May require multiple sessions
- Electrocautery or Radiofrequency Ablation
- Destroys warts using electric current or radio waves.
- Performed under local anesthesia.
Best for: Stubborn or thick warts
Benefits: Quick results, minimal downtime
- Laser Treatment
- Uses CO₂ laser to precisely vaporize wart tissue.
- Ideal for large or difficult-to-treat warts.
Advantages: High precision, minimal scarring
Cost: Typically, higher than other methods
- Surgical Excision
- Involves physically cutting out the wart under local or general anesthesia.
- Usually reserved for large or obstructive warts.
Benefit: Immediate removal
Consideration: May require stitches and post-procedure care
Genital Warts During Pregnancy
Warts may grow more rapidly during pregnancy due to hormonal changes. Some treatment options like cryotherapy or laser therapy are considered safe during pregnancy. However, many dermatologists prefer to delay treatment until after delivery unless symptoms cause significant discomfort or complications.
Important Precautions
- Do not use over-the-counter wart removers meant for hands or feet on genital areas, as they can severely irritate or damage sensitive skin.
- Never self-treat genital warts without medical advice.
Can Genital Warts Recur?
Yes. Since HPV can remain dormant in the body, warts can recur, particularly if the immune system is weakened. Consistent follow-up and, in some cases, maintenance treatment can reduce the risk of recurrence.
Preventing Genital Warts
- HPV Vaccination
The HPV vaccine (Gardasil 9) is the most effective preventive tool. It protects against:
- Low-risk HPV types 6 and 11 (genital warts)
- High-risk types 16, 18, and others (cancers)
Recommended for:
- Boys and girls aged 9 to 26
- Adults up to 45 years (based on doctor’s advice)
- Safe Sexual Practices
- Use condoms consistently (though not 100% effective in preventing HPV)
- Limit the number of sexual partners
- Avoid sexual contact with anyone who has visible warts or known HPV
- Get regular STI screenings
When to See a doctor
Consult a specialist if you:
- Notice any unusual growths or bumps in the genital area
- Experience itching, discomfort, or bleeding
- Are pregnant and have warts
- Have a history of HPV or abnormal cervical screening results
Conclusion
Genital warts are common but manageable. With early diagnosis, expert care, and preventive strategies like HPV vaccination and safe sex practices, individuals can control outbreaks and protect themselves and their partners. Though there’s no permanent cure, modern dermatological treatments offer effective options for genital wart removal and symptom relief.